News and Insights
From Co-Pays to NHS Delays – a Comparative Prognosis of US, UK and Republic of Ireland Health Systems
May 20, 2025
The Perspective of Three Global Health Communicators on Access to Care
As a dual citizen of Ireland and the UK, my trusty blue Ventolin inhaler frequently accompanies me on my travels across the border, even while I lived and worked in the United States for a few years, to manage my asthma. My local British supermarket, ASDA, stocks this inhaler at £14.00. In Ireland, the receipt prints €23.00 at a McCabes Pharmacy, while the Walgreens in my old neighborhood in New York priced my breathing aid at around $33. The price of medication is mediated by insurance in all three countries. Still, these systems are constantly shifting in favor of, and sometimes against, the better interests of patients.
A patient-centric approach is the common denominator of most global health systems. Yet, my personal experiences suggest that patients must manage their conditions and expectations when faced with conflicting health insurance frameworks. More than 28 million people have asthma in the US (Asthma and Allergy Foundation of America), along with 7.2 million people in the UK (Asthma + Lung UK), and 460,000 people in Ireland (Asthma Society of Ireland), which equates to one of the highest asthma rates per population globally.
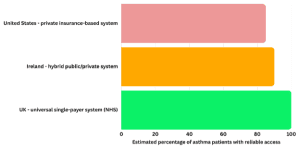
In the UK, an estimated 95-100% of asthma patients have universal, free, or low-cost access to medication through the NHS. In Ireland, 75-90% of asthma patients may access the same medication for free using a medical card, or by an out-of-pocket scheme capped at $80 per month. In the US, this figure drops to 75-85%, with underinsured patients unable to afford the higher costs of medications, and those without insurance unable to access treatment.
Asthma is not the only condition where price variation has an impact on the lives of patients. We can see echoes of this in the rising popularity of weight-loss medications, with global organizations navigating accessibility, affordability, and supply across global markets. A weight loss drug manufacturer must consider the availability and price of their product, as well as its availability to patients depending on their insurance coverage, across international markets. Translating the needs of the patients, and taking into account the national insurance and general taxation funded schemes versus private insurance framework, thus requires knowledge of the health landscape, which is becoming increasingly complex in the wake of changes across the US, UK, and Europe.
Working for organizations and patient communities means fighting anti-social socialized health systems. How can we craft campaigns around services or products most patients cannot access due to their insurance coverage, or against rising subsidized costs from national health systems or providers?
According to a 2025 Global Medical Trends Survey by WTW, 64% of insurers anticipate higher or significantly higher medical trends globally over the next three years, with two-thirds (67%) anticipating higher or significantly higher global demand for health services, most notably in Europe. As such, health insurance is becoming a perk rather than a standard provision.
In seeking answers to these questions, I sought the opinion of three FINN Partners’ Global Health Practice leaders with experience driving patient-centric campaigns across diverse international landscapes.
“It’s about the health of the system, not the health of society,” says Gil Bashe, Managing Partner, Chair Global Health and Purpose, FINN Partners. “The United States leads in medical innovation—from breakthrough therapies to cutting-edge technologies—but access to that innovation remains elusive for too many. We have an ecosystem that rewards invention, yet often overlooks the individual. Millions still face barriers to care due to cost, coverage gaps, or system complexity. In a nation rich with health possibilities, no one should be left navigating whether they can afford wellness. In an ideal world, wellness costs less than disease—but until access is prioritized alongside innovation, that ideal remains out of reach.”
A significant change to the US health market may come from the most recent update from President Trump’s administration. Having signed the executive order for the “Most-Favored-Nation” pricing policy, which aims to change the pricing, assessment, and development of medicines across the world market, President Trump is mandating that the US will not pay more for a pharmaceutical product than the lowest price it is sold for in any other country.
As insurance providers race to amend their policies for paying customers, the communication professionals they consult are now tasked with navigating emerging changes to the health system in real time and implementing subsequent thinking in communication strategies to benefit the communities we and our clients want to serve.
With obesity cases rising and mental health issues impacting communities on a staggering level, for example, health companies must promote resources that address the stem of the problems, from nutritional education to accessible mental health support. By providing these organisations with vital tools to communicate to patients and communities, we are creating opportunities for wellness at the earliest stages that would prevent patients, in most cases, from requiring costly and unsustainable treatment options.
The drive for patients to be cared for beyond the parameters of hospitals has recently sparked calls for reform to Ireland’s two-tier health system, with the newly proposed Sláintecare strategy designed to provide a universal health system to Irish citizens, much like the NHS. The current “pay-per-visit system” that many Irish citizens have become accustomed to, Christopher Nial, Senior Partner, EMEA Public Health, explains was designed to minimize strain on the health system while balancing the coverage costs for all. A visit to an urgent care facility may set you back €80 – not quite enough to deter a broken arm, but enough to reconsider a runny nose.
However, the shift towards accessible health is a key driver of Ireland’s new health vision. A recent article penned by Christopher highlights the noticeable gains of countries investing in “universal public services, fair taxation policies, robust labour rights, and social protection”. To that extent, Christopher comments, “[w]ell-being budgets, if undertaken properly, represent a way to begin to move past the obsession with GDP, and consider what matters.” It seems that Ireland may be adopting a system that mitigates and curbs, rather than deters, high-demand services for the benefit of its citizens.
As a steadfast institution of health, the NHS is a core part of the UK’s infrastructure, becoming as entrenched in socio-political and economic debate as the countries it serves. Julian Tyndale-Biscoe, Senior Partner, UK Health, recently addressed the abolition of NSHE (NHS England) as a “major challenge” in the wake of technological advancements, organizational structure, and general workforce stability of the NHS.
Sudden changes to the structural integrity of the NHS could significantly impact the number of UK-based individuals opting for private insurance, which nearly doubled between 2019 and 2022 according to data from Statistica’s Consumer Insights. With almost one in eight people in the UK having private medical insurance, the shift to private health is driven by desperation to reduce prolonged waits for time-sensitive surgeries, with hospitals seeing little decline in emergency waiting room times and increased pressure on the NHS workforce.
The UK must continue to prioritize universal health while concentrating on maximizing public resources. By encouraging patients to use free health services and utilizing customized resources developed by communication experts in the health space, the pressures on the NHS may be alleviated without sacrificing its defining role as a health provider.
It’s reassuring to know that expert teams stand behind the innovations shaping care for a growing spectrum of health conditions. Yet expertise alone is not enough. Global health organizations – biotech, pharma, and health systems – must develop strategies tailored to the diverse markets they serve—strategies that balance innovation with accessibility and affordability. As disparities persist across health systems in the US, UK, and Ireland, the role of health communicators becomes more critical than ever. We are not just storytellers, we are advocates. It is our responsibility to elevate patient-centric strategies, challenge systemic inequities, and help build the trust and clarity needed to advance healthier, more equitable communities.
