News and Insights
The Neurological and Emotional Power of Stories in Health
June 17, 2025
Health is more than a clinical transaction; it is one of the most emotionally resonant human experiences, marked by uncertainty, vulnerability, hope, and often, profound transformation. Yet, despite the sector’s reliance on evidence, data, and protocols, one of its most powerful tools remains profoundly human and ancient: the story, a science-led art that is not used by the health industry to its fullest potential.
During the last two decades as a communications professional consulting global companies across pharmaceuticals, medical technologies, health providers, diagnostics, or public health campaigns, one truth has become increasingly clear: storytelling is not just a communication technique. It is a biological, neurological, and emotional mechanism that can bridge gaps no statistic ever could.
And in a world grappling with medical mistrust, misinformation, and mental health pandemics, understanding why stories work, especially in health, is no longer optional. It is strategic, ethical, and essential.
The Brain on Story: A Neurological Primer
Neuroscientists have long studied the impact of storytelling on the brain, and their findings are compelling. When we hear facts, only the brain’s language processing centers—Broca’s and Wernicke’s areas—are activated. But when we hear a story, especially one rich in emotion and sensory detail, a far broader neural network comes alive.
According to neuroeconomists, compelling narratives trigger the release of oxytocin, the “empathy hormone.” This biochemical change fosters trust and emotional resonance. Research has shown that people are more likely to donate to a cause, adhere to health protocols, or change behavior if the communication is story-driven and emotionally immersive.
In healthcare, this has immense implications—from improving patient adherence to enhancing doctor-patient empathy to humanizing public health campaigns.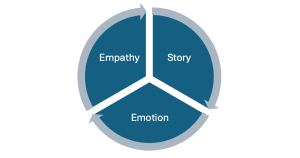
The “S.E.E.” Framework: Why Health Stories Stick
To unpack how storytelling exerts such a powerful hold in health communication, let us consider, S.E.E. Framework—Story, Emotion, Empathy.
- Story
Stories provide structure to chaos. A diagnosis like cancer or an ICU admission is often overwhelming. Stories give these events a narrative shape: a beginning, a crisis, a struggle, and sometimes, a resolution. This structure helps both the narrator and the listener make meaning out of suffering. - Emotion
Clinical information may inform, but emotion compels. Health narratives with emotional content are remembered up to 22 times more than facts alone (per cognitive psychologist Dr. Jennifer Aaker, Stanford GSB). Whether it’s a caregiver’s struggle or a survivor’s hope, emotion becomes the mnemonic anchor. - Empathy
Stories build what philosopher Martha Nussbaum termed “empathic imagination.” They allow policymakers to see beyond budgets, doctors to feel beyond diagnoses, and the public to understand beyond headlines. It’s no accident that narrative medicine is now a core module at Columbia University’s medical school.
Case in Point: When Data Met Drama
In 2020, during the peak of the COVID-19 pandemic, Singapore’s Ministry of Health launched a campaign called “Behind the Mask,” which featured nurses and ambulance drivers narrating their lived experiences. Instead of broadcasting case numbers or logistical updates, the campaign leveraged first-person storytelling.
The result? The campaign achieved 3X higher engagement than traditional PSAs, helped reduce stigma against health workers, and was cited in behavioral research journals as an exemplar of “emotionally intelligent public health.”
Another standout is the “Touching Lives” series from Apollo Hospitals in India, featuring patient stories that improved online consultations and drove measurable increases in preventive health screenings across tier-2 cities.
Not Just Soft—Strategic
There is a tendency in boardrooms and bureaucracies to view storytelling as ‘soft.’ That’s a strategic oversight. McKinsey’s “Voice of the Customer” studies show that emotionally engaged patients are 3.5x more likely to follow treatment plans. Pharmaceutical companies using story-based patient journeys see higher HCP recall rates by 40% compared to traditional detailing.
This isn’t branding fluff. It’s a neuroscience-backed behavioral design. Moreover, in advocacy, stories have swayed more policies than white papers.
Ethics and the Edge
But with great emotional power comes ethical responsibility. Health stories must protect privacy, avoid manipulation, and center dignity. The best storytellers in health are not the ones who say the most, but the ones who listen deeply, translate responsibly, and amplify wisely.
As health systems become more digital, data-driven, and AI-augmented, the human need for connection doesn’t diminish; it deepens. Stories, when crafted with integrity, can bridge systemic gaps, rebuild trust, and turn information into inspiration.
In the future of health, where algorithms will guide diagnosis and robotics may assist surgery, stories will still do what they have always done best: heal, humanize, and connect.
And if we want to truly transform global health systems—not just technologically, but emotionally and culturally—we must first learn to see through the patient’s eyes, feel with their heart, and walk a mile in their story.
